A Brief History of Vaccines: an endless war between humans and pathogens
It all started with smallpox, one of the deadliest diseases in human history. The earliest cases of smallpox can be dated to 1350 BCE in ancient Egypt, with the evidence found in Egyptian mummies. Only until the late 20th century when smallpox was eradicated entirely, this horrible disease tormented the human population for thousands of years. Smallpox is a disease caused by the infection of variola virus. This virus killed 1/3 of the people infected, and among the people who survived the illness, it left marks on their faces and bodies. There is no cure today. Therefore, the attempts of preventing smallpox initiated the development of vaccines.
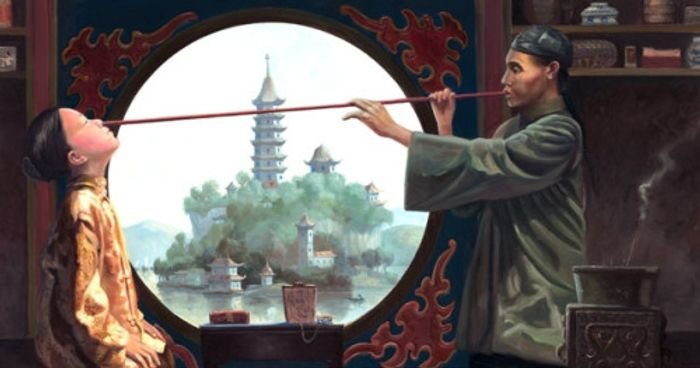
1695-1721: Early attempts
The earliest attempts at smallpox inoculation were documented in an ancient Chinese medical text The Golden Mirror of Medicine. To prevent the uninfected from contracting smallpox, medical practitioners collected scabs from smallpox patients, then dried and ground the scabs. The powered scabs were blown into the patient’s nose. Such practice meant to introduce a small amount of agent that caused smallpox (now known as variola virus) to induce immunity against smallpox in healthy individuals. It usually only caused a milder form of illness in the recipients.
In 1721, Lady Mary Wortley Montagu, who survived smallpox yet was unfortunately disfigured by the disease, first introduced variolation in Europe. During her trip to Turkey in 1717, Lady Montagu observed a different form of variolation. She saw a doctor inject dried pus from smallpox pustules into the skin of a patient in Turkey. After her return to England in 1721, Lady Montagu had Dr. Charles Maitland perform variolation on her daughter, marking the first variolation in Europe.
Variolation in general was effective against smallpox if successful, yet 2-3% of patients treated died of smallpox. Due to the danger of contracting smallpox from variolation, this technique wasn’t widely accepted in the world. A safer method to prevent smallpox was still needed.
1774-1801: Benjamin Jesty, and Edward Jenner
In 1774, Benjamin Jesty, a cattle breeder in England, first noticed his immunity to smallpox after contracting cowpox from his herd. Cowpox is now known as a virus that’s closely related to smallpox, but it only causes mild illness in humans. Then, based on his observation, Jesty inoculated his wife and two children with cowpox. Jesty’s experiment was successful, his family was not affected during the outbreak of smallpox. However, neither a scientist nor a physician, Jesty’s successful vaccination story didn’t spread far.
Edward Jenner also noted this village folklore when he was an apothecary apprentice in Chipping Sodbury, England in 1768. This story inspired him to study the association between cowpox and smallpox during 1770-1773. Yet, for some unknown reason, he didn’t test the protective effects of cowpox until 1796 when he inoculated 8-year-old James Phipps with cowpox. Two months after the inoculation, Jenner inoculated Phipps again but this time with a smallpox lesion from a patient. No disease developed.
Image of Edward Jenner from British Medical Journal
This groundbreaking result didn’t spark public interest in receiving Jenner’s cowpox vaccine. In fact, rumor had it that the cowpox vaccine would turn people into cows (sounds familiar?). The public’s trust in Jenner’s vaccine was slowly built when an extensive study was carried out and the efficacy of this vaccine was proven in a larger population.
People believed Jenner’s smallpox vaccine would turn them into cows. Image from the WHO: History of the smallpox vaccine.
1873-1885: Live attenuated vaccines by Louis Pasteur and Henry Toussaint
In 1879, Louis Pasteur was trying to create a weaker chicken cholera (Pasteurella multocida), by passaging from chicken to chicken. But this method was unsuccessful because the strain of chicken cholera was very virulent, and most of the chickens fell dead after inoculation of chicken cholera. In July 1879, Pasteur went on a vacation and left the chicken cholera culture unattended. After he came back from vacation in October, Pasteur resumed his research. He realized that after leaving the chicken cholera culture in an acidic environment for 4 months, the chicken cholera became less virulent. In 1880, he immunized 8 chickens with this “attenuated” chicken cholera and compared it with other 19 chickens that were never immunized. All 8 previously immunized chickens lived, whereas most of the unimmunized chickens did not survive.
Pasteur used aged chicken cholera culture to immunize chickens. Image from Veterian Key
In 1873, Henry Toussaint also independently discovered ways to produce attenuated vaccines for anthrax. He collected blood from sheep infected by anthrax and treated it with heat or phenol acid, a bactericidal chemical. All 22 sheep immunized with either heat-treated or phenol-treated vaccines survived the lethal anthrax challenge.
Pasteur and Toussaint’s work with chicken cholera and anthrax started the new era of standardized attenuated vaccine production. And animal tests became a common approach to test the safety of vaccines.
In 1885, Pasteur used a similar approach to create a rabies vaccine for treating Joseph Meister, a 9-year-old boy attacked by a rabies dog. This method successfully saved the boy from contracting rabies. It was the first case of post-exposure vaccination treatment. Yet, this practice was not celebrated by the medical community, rather the fact that Pasteur injected a human patient with a lethal pathogen provoked controversy.
1884-1891: Immunology in vaccine development
In the early days, vaccine development was purely empirical. Scientists didn’t know how vaccines induce immunity against pathogens until 1884 when Ilya Mechnikov reported his seminal work on phagocytes, which he called macrophages. In his theory, Mechnikov described these cells ingested and destroyed invading microorganisms and other foreign bodies. This work may be the first observation of how immune reactive molecules (e.g. proteins and polysaccharides) from pathogens or vaccines, now known as antigens, are presented to the immune system.
Ilya Mechnikov and his drawing of macrophages. Image from Nature Immunology.
In 1888, Emil von Behring found that serum from animals previously injected with a sublethal dose of diphtheria toxins can neutralize the toxin in culture. Later, von Behring observed that if he injected the serum from animals previously immunized with diphtheria toxin into animals sick from diphtheria, the serum could cure the symptoms. Based on his result, he thought a low dose of diphtheria toxin can make the animals produce what he called “antitoxins” in the blood, and the antitoxins can protect the animals from illness caused by diphtheria. In 1889, von Behring successfully used diphtheria antitoxin to treat a child suffering from diphtheria infection. Such success allowed von Behring to commercialize his serum product from rabbits immunized with diphtheria toxin.
Now we know the antitoxins that neutralized diphtheria toxin were antibodies. But this term was not created until Paul Ehrlich worked on his theory of how antibodies are produced when the immune cells encounter foreign antigens.
Paul Ehrlich and his drawing of cells producing antibodies. Image from Nature Immunology.
These groundbreaking findings set the foundation for the knowledge we use to develop modern-day vaccines. von Behring was awarded Nobel Prize in Medicine in 1901, and Ehrlich and Mechnikov shared the Nobel in 1908.
1918-1952: Spanish flu, flu vaccine, and the Global Influenza Surveillance and Response
Beginning in 1918, the influenza pandemic swept across the world. About 500 million people or 1/3 of the entire human population were infected, claiming at least 50 million lives between 1918 and 1919. That is more than 7 times the cumulative deaths, 6.8 million, caused by COVID-19 when this article was written. Retrospective studies proved H1N1 influenza A virus was the culprit of this pandemic, but at that time scientists didn’t even know it was caused by a virus. Influenza or flu was first thought caused by bacteria until Wilson Smith, C.H. Andrewes, and P.P. Laidlaw at London’s National Institute for Medical Research first isolated and identified the influenza virus from patients. This finding drastically accelerated the development of the flu vaccine, leading to the first flu vaccine for wide use in 1945.
Emergency hospital during the influenza pandemic, Camp Funston, Kansas (1918). Image from National Museum of Health and Medicine.
Scientists later found that there was more than one strain of influenza A virus, and they also isolated a different influenza virus, named influenza B virus, that usually only causes mild symptoms. In response to multiple strains of influenza A and B viruses, World Health Organization (WHO) established the Global Influenza Surveillance and Response System (GISRS) in 1952. WHO monitors the influenza virus strains circulating in different parts of the world. And based on the surveillance, WHO each year recommends virus strains for inclusion in flu vaccines for each hemisphere, targeting 3 or 4 strains of the virus predicted to be most commonly circulating in the coming flu season.
1959-1980: Global collaborative effort to eradicate smallpox
Despite the availability of smallpox, this disease continued to be a major threat to public health in the first half of the 20th century. The worst outbreak was in 1949, more than 600,000 people were infected. In order to eradicate smallpox once and for all, the WHO orchestrated the Smallpox Eradication Program in 1959 to expand the smallpox vaccination to the global level. And the Intensified Smallpox Eradication Program was launched in 1967 with The Soviet Union providing vaccines to eastern Europe, China, and India. Such an effort was a huge success, smallpox was eliminated from South America in 1971, Asia in 1975, and Africa in 1977. Following the last 2 cases of smallpox identified in 1978, WHO in 1980 announced smallpox has been completely eradicated, marking one of the greatest triumphs against infectious diseases in human history.
Global smallpox cases. Grey lines indicate the initiation of the Smallpox Eradication in 1959 and the Intensified Smallpox Eradication Program in 1967, respectively. Data from WHO (2011).
1986: Vaccine safety and subunit vaccines
Vaccines containing attenuated pathogens (e.g. measles, mumps, and rubella (MMR) vaccine) or killed pathogens (e.g. Havrix, an influenza A vaccine) were effective in inducing immunity in vaccinees. Yet, the side effects of whole-pathogen vaccines started to become a concern to the public as infectious diseases became less of a threat in the 1970s. The reduction of vaccination coverage caused outbreaks during that time. Therefore, a safer vaccine strategy was needed to regain public trust.
Due to the advances in laboratory techniques in the era of genetic engineering in the 1970s. Subunits of pathogens, usually a crucial protein or other molecules for their infectivity and/or virulence, were able to be produced in large quantities from cell culture. As opposed to whole-pathogen vaccines, subunit vaccines only contain parts of the target pathogen and hence are much safer. Pablo Valenzuela in 1982 first mass-produced surface antigen of hepatitis B virus from yeast culture, leading to the licensing of the first subunit vaccine in 1986. Since then, subunit vaccines became the trend of vaccine strategies.
Despite their superior safety profile, the biggest caveat of subunit vaccines is their poor immunogenicity— subunit vaccines are not as effective in activating immune responses. Because subunit vaccines don’t have the features of real pathogens or whole-pathogen vaccines. Immune cells rely on these features to recognize them as pathogens before they initiate immune responses. Therefore, an extra component to help alert the immune system to target the antigens in subunit vaccines became important for this type of vaccines. Such agent is called an adjuvant. Thus far, 6 adjuvants have been approved to use in vaccines in the United States.
The increased use of adjuvants in licensed vaccines when subunit vaccines began to gain popularity after 1986. Image from Di Pasquale et al. in Vaccines.
1987-the 2010s: The formidable challenge of HIV vaccine and the advent of structural vaccinology.
The first cases of human immunodeficiency virus or HIV were reported in the United States in 1981 among young gay men with severely damaged immune systems. There was no cure for those diagnosed with this deadly virus—74% of them would die within 10 years after diagnosis. As a vaccine against HIV became desperately needed, the first HIV vaccine trial was launched in 1987. Unfortunately, the unparalleled speed of mutation in HIV poses a major hurdle for vaccine designs against this notorious virus. Even 40 more years after the first outbreak and many failed trials, there is still no effective HIV vaccine available today.
Yet, the formidable challenge of HIV vaccines galvanized vaccinologists to take on new approaches. At that time, structural biologists already knew how to use X-ray crystallography and cryo-electron microscopy to analyze protein structures at atomic levels. Therefore, using these technologies to analyze antigens from pathogens became a new trend for vaccine designs. Today, structural vaccinologists can identify the sites of vulnerability in a virus and engineer vaccines to target those sites by analyzing how the virus is neutralized by antibodies from patients who have recovered from an infection or have an ongoing infection.
The approach of structural biology for vaccine designs. Image from Frontiers in Microbiology by Mohd Ishtiaq Anasir and Chit Laa Poh.
2000-the 2010s: Applying nanotechnology to vaccine development
In early 2000, nanotechnology started to burgeon and became a new realm of science. Along with the advancement of our understanding of the immune system, some scientists realized that nanomaterial can also be used to deliver antigens in vaccines and enhance desired immune responses. John Schiller among other pioneers used virus-like particles, a class of nanoparticles utilizing virus proteins for the scaffold of the nanoparticles, to deliver antigens. Schiller found that presenting antigens in an array on virus-like particles can drastically increase the immune response to those antigens. That is because the repetitive pattern of protein on a particle is a signature of pathogens, and the immune system is hard-wired to respond to that pattern. Therefore, presenting antigens on nanoparticles like the way on an actual virus or other pathogens enhances the immunity against the target pathogen.
Other than changing the way antigens are presented, different nanomaterials have been used to deliver antigens to specific cells, to deliver both antigens and adjuvants together, to protect nucleic acid (DNA or RNA) vaccines from degradation, and more.
Schematic (left) of an HIV vaccine, where HIV envelope antigens are presented on a ferritin nanoparticle; and the image of this vaccine under a transmission electron microscope (right). Images from Science by Talar Tokatlian et al.
The 2020s: Nucleic acid vaccines
Although subunit vaccines have been proven safe, the manufacturing of subunit vaccines usually involves live cell culture for producing antigens, which can be time-consuming and costly. So, it is challenging for subunit vaccine production to keep up with the constant emergence of new pathogens or the re-emergence of known pathogens. Therefore, safe, cost-effective, and less time-consuming vaccine strategies were needed to prepare the world for the potential outbreaks of pathogens. Vaccinologists started to test nucleic acids in the 1990s and early 2000. Unlike subunit vaccines, the production of nucleic acid vaccines does not involve cell culture, so the production is much faster and cheaper. And numerous animal tests also demonstrated the safety profile of nucleic acid vaccines.
When a virus or other pathogen infects a cell, it turns the cell into a factory to produce its own proteins to reproduce itself. The pathogen first delivers its nucleic acid (can be DNA or RNA) to hijack the cell’s protein production machinery, then the cell starts to make the pathogen’s proteins by following the instructions in the nucleic acid. Similar to the actual pathogen, nucleic acid vaccines also deliver the pathogen’s nucleic acid to the cells. However, nucleic acid vaccines only contain the piece of nucleic acid for a pathogen protein that serves as an antigen to activate immune responses. Therefore, like subunit vaccines, there is no chance for nucleic acid to cause infection.
In early 2020, COVID-19, a respiratory disease caused by the SARS-CoV-2 virus, swiftly spread to every country in the world. In January 2020, COVID-19 was declared a Public Health Emergency of International Concern by WHO, with an official death toll of 171. By the end of 2020, this figure stood at over 1.8 million. In the face of the pandemic, the world was crying out for vaccines that can be quickly produced and dispatched to every corner of the world. Thanks to the decades of research before the pandemic, the first nucleic acid vaccines for COVID-19 were quickly manufactured and approved in the same year for emergency use by the FDA of the U.S. and other countries.
Shanghai under city-wide lockdown in March 2022. Image from BBC News.
There are two types of nucleic acid vaccines, DNA and messenger RNA (mRNA). DNA vaccines are usually more stable but to make the cell produce antigens, DNA must travel to the cell nucleus first. So, to help a DNA vaccine deliver to the cell nucleus, innocuous viruses such as adenoviruses are usually used as a vector. The DNA vaccines manufactured by AstraZeneca (U.K.), Johnson & Johnson (U.S.), and Sputnik V (Russia) are delivered by adenoviruses.
An mRNA vaccine does not have to travel to the cell nucleus to make the cell produce antigens, it can make antigens while in the cytoplasm. Yet, mRNA vaccines are much less stable than DNA because the enzyme known as RNase that digests RNA molecules is present in body fluid. Therefore, lipid nanoparticle (LNP) is used in the mRNA vaccines developed by Pfizer-BioNTech (U.S. and Germany) and Moderna (U.S.) to protect mRNA from RNase before it is delivered to the immune cells.
In COVID-19 nucleic vaccines, RNA and DNA of the SARS-CoV-2 spike protein are packaged in lipid nanoparticles and adenovirus vector, respectively. Image grafted from Military Medical Research by Dan-Dan Li & Qi-Han Li.